Bacterial Vaginosis or BV
Online treatment for bacterial vaginosis
Get treated online
Topics we’ll cover
Reviewed by Tami H., CNP for Virtuwell
Bacterial vaginosis (also known as BV), is a common type of vaginal infection that can develop when your vagina’s normal bacterial flora becomes unbalanced. If this happens, you may develop an infection and experience some uncomfortable symptoms. The good news is that BV can easily be treated. Keep reading to learn more about BV and how Virtuwell can help you get your vaginal microbiome back in balance.
Signs & symptoms
What does B.V. look & feel like?
Some people who have BV experience symptoms, but many do not. In fact an estimated 84% of people with BV have asymptomatic bacterial vaginosis and don’t notice any symptoms. If you do have symptoms, they can be mild or severe and may be more noticeable after sex or around the time of your period.
Common BV symptoms
-
Vaginal discharge that is a thin consistency and gray or off-white in color
-
Strong fishy vaginal odor
-
Vaginal irritation
Could it be something else?
Many BV symptoms overlap symptoms associated with STIs. So if you’re sexually active and there’s a chance you could have a STI, it’s a good idea to get tested. Getting tested for common STIs like chlamydia, trichomoniasis and gonorrhea can help you get to the bottom of what’s causing your vaginal discomfort and ensure you get the treatment you need to start feeling better.
At-home STI testing
Concerned you have a STI?
Similar conditions we treat
Whether you have BV or a STI, our nurse practitioners can diagnose and treat you online — all from the comfort of your home. Plus, if you have any questions or concerns, follow-up care is free.
Causes & risk factors
How do you get bacterial vaginosis?
Your vagina naturally contains numerous strains of bacteria and, when the normal ratio of that bacteria becomes unbalanced, you can develop a common type of infection known as bacterial vaginosis or BV.
According to the Centers for Disease Control and Prevention (CDC), BV is the most common type of vaginal infection among women ages 15 to 44, and an estimated one-third of people with vaginas will develop BV at some point during their lifetime – some numerous times. While it’s unclear why some people develop BV, certain activities have been identified as risk factors that can increase your chances of getting BV.
BV risk factors
-
Sex with multiple partners
-
Sex with new partner(s)
-
Unprotected sex
-
Smoking cigarettes
-
Having an IUD
-
Douching


While sex is a risk factor in developing bacterial vaginosis, BV is not a sexually transmitted infection (STI). And people who haven’t had sex can develop BV too.
—Tami H., CNP for Virtuwell
If you think you may have BV, it’s important to seek medical treatment. If left untreated, BV can increase a person’s risk of getting and transmitting STIs including HIV, chlamydia and gonorrhea. It can also increase the risk of developing pelvic inflammatory disease – a painful infection that can cause scarring in the reproductive system, making it hard to get pregnant.
If you are pregnant and think you have BV, it’s important to let your doctor know so you can get treatment. Pregnant women who have BV are at an increased risk of experiencing complications including preterm delivery and delivering babies with low birth weight.
Treatment options
How do you get rid of bacterial vaginosis?
The only sure way to clear up a BV infection is with a prescription antibiotic. A medical provider may prescribe an oral antibiotic or an antibiotic in vaginal suppository form – both pill and suppository antibiotics effectively kill the bacterial strains that cause a BV infection. The type of antibiotic prescribed will depend on your symptoms, medical history and personal preference.
Virtuwell treats BV online every day
-
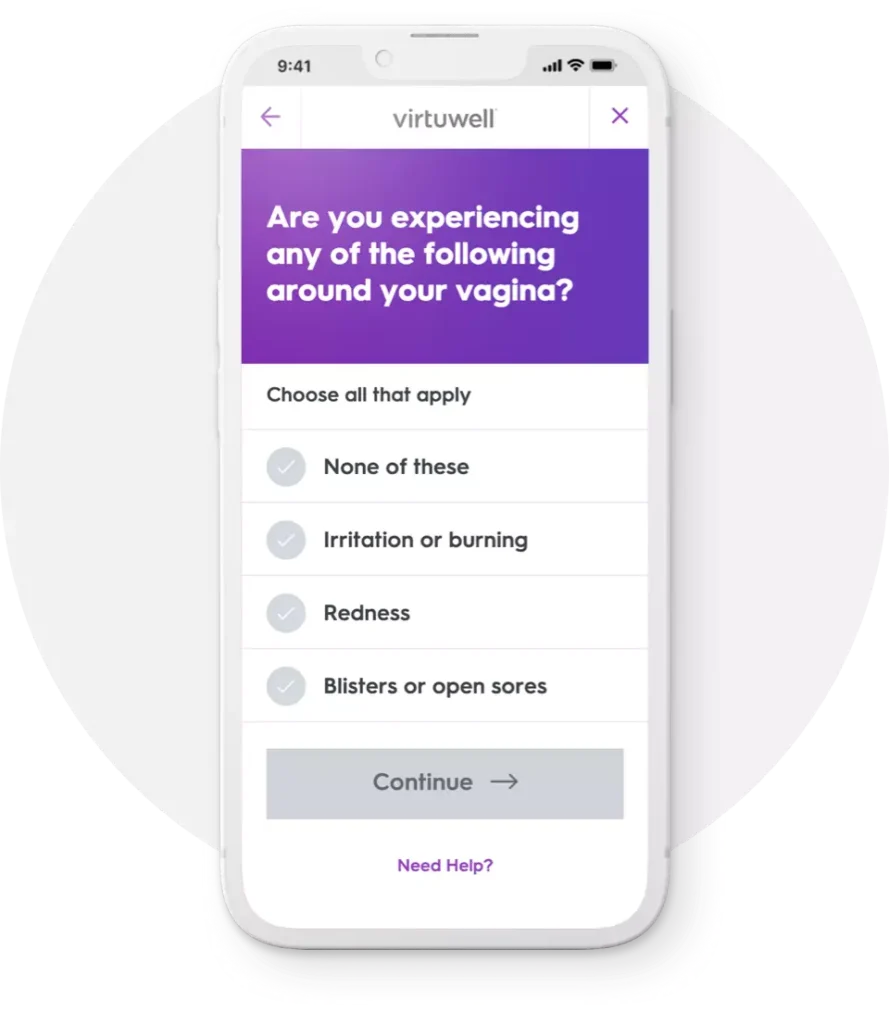
Tell us about your symptoms
A simple questionnaire helps us understand more about how you’re feeling.
-
Quick diagnosis by an expert
A certified nurse practitioner reviews your answers and tailors a treatment plan to your symptoms.
-
Treatment plan and prescriptions
A text and email are sent to you when your plan is ready. If needed, we’ll send prescriptions to your pharmacy.
A Virtuwell visit is $0-79 with insurance
Your visit includes a diagnosis, treatment plan, prevention tips and follow-up care.
BV prescription medications
Two of the most commonly prescribed antibiotics for BV are metronidazole and clindamycin. If you are prescribed an antibiotic, your symptoms will likely begin to improve within a couple of days of starting the medication. Even if this happens, it’s very important that you continue to take the full course of antibiotics. If you don’t take all of your prescribed medication, your infection may not fully resolve and could come right back. You could also experience complications related to antibiotic resistance.
Metronidozole
Commonly-prescribed antibiotic to treat BV. Comes in both oral and topical cream forms.
Clindamycin
Less-commonly prescribed antibiotic. Typically prescribed as topical cream to treat BV symptoms.
In addition to taking all of your prescribed medication, it’s also a good idea to avoid having sex until your infection completely clears up.
Unfortunately, an estimated 50% of people who get BV once will develop subsequent infections within 12 months. If you are age 26 or older, you can get treated for BV online through Virtuwell.
Simply start Virtuwell visit for BV and tell us about your symptoms. We’re here to answer your questions about recurrent bacterial vaginosis and provide treatment to help you feel better fast.
Convenient anywhere care
Get BV treatment now
Home & self-care tips
Can you treat bacterial vaginosis at home?
Sometimes BV goes away on its own. However, because BV is an infection, you need a prescription antibiotic to clear it up and resolve the root cause. If you have symptoms and think you may have BV, it’s a good idea to seek medical treatment.
Prevention tips
How can you prevent bacterial vaginosis?
While extremely common and treatable, most people want to do everything they can to avoid getting bacterial vaginosis. And even though there’s no way to prevent BV with 100% certainty, there are things you can do to reduce your risk of an infection.
Common question
Answers to common questions about bacterial vaginosis
- Is bacterial vaginosis a STI?
-
No, bacterial vaginosis is not a sexually transmitted infection. While sex is considered a risk factor in developing BV, you can get BV even if you’ve never had sex. In truth, anything that disrupts your vagina’s natural PH balance is considered a risk factor in developing BV. This includes having sex – especially multiple sex partners – but also things like douching and even getting your monthly period.
- Can people with penises get BV?
-
Only people who have vaginas can get BV. However, both people who have vaginas and people who have penises can develop and pass along sexually transmitted infections (STIs) to their partners. And symptoms associated with BV can overlap with symptoms associated with common STIs like chlamydia and gonorrhea.
If you’re sexually active, take steps to protect your sexual health. Get an at-home STI test kit online today. Knowing your STI status, can help ensure you get the best and most-effective treatment for your symptoms.
- Is BV contagious?
-
No, BV is not something that can be spread from person to person. However, you are at a greater risk for developing BV if you’re sexually active and your risk increases the more sexual partners you have. Women who have sex with other women are also at a greater risk for developing BV.
- Can you have sex while you have BV?
-
If you have BV, it’s recommended that you don’t have sex until you complete treatment and your infection completely resolves. Standard treatment for BV includes taking an antibiotic – either an oral or suppository medication – for 3 to 7 days. If you continue to experience symptoms after taking all of your medication, continue to avoid sex and reach out to a medical provider for advice on next steps.
- Why do I keep getting bacterial vaginosis?
-
Unfortunately, some women are prone to developing BV. And if you have BV once, you’re more likely to get it again. There’s no way to definitively prevent BV. However, you can reduce your chances of getting BV by knowing and taking steps to avoid or reduce identified risk factors.
- Is bacterial vaginosis a yeast infection?
-
Symptoms associated with BV and yeast infections – including changes in vaginal discharge – can overlap. However, BV is not a yeast infection and vice versa. Therefore, medications used to treat yeast infections will not effectively treat BV – this includes prescription medication.
To ensure you get the correct and most-effective treatment for your specific health issue, it’s wise to seek the advice of a medical provider. Based on your personal history and symptoms, a provider can help determine the root cause of your vaginal discomfort and provide a treatment plan and – if needed – prescription medication to help you feel better.
- Can bacterial vaginosis cause pain?
-
Women who get BV may experience vaginal swelling and general discomfort. While uncomfortable, these symptoms should not be painful. If you are experiencing pain in your vaginal or abdominal region, it’s important to seek medical attention at an urgent care clinic or emergency room department.

